Case Report | Vol 11 | Issue 2 | May-August 2025 | Page: 11-16 | Ashish Nair, Jerry Mathew, Athira CN
DOI: https://doi.org/10.13107/jaccr.2025.v11.i02.276
Open Access License: CC BY-NC 4.0
Copyright Statement: Copyright © 2025; The Author(s).
Submitted: 15/02/2025; Reviewed: 11/03/2025; Accepted: 24/06/2025; Published: 10/08/2025
Author: Ashish Nair [1], Jerry Mathew [1], Athira CN [1]
[1] Department of Anaesthesiology & Critical Care Medicine, Bharti Vidyapeeth Hospital, Pune, Maharashtra, India.
Address of Correspondence
Dr. Ashish Nair,
Department of Anaesthesiology & Critical Care Medicine, Bharti Vidyapeeth Hospital, Pune, Maharashtra, India.
E-mail: ashishnair1991@gmail.com
Abstract
A 5-month-old child presented with high-grade fever with cough, and noisy breathing to the EMD. On evaluation, the baby appears to have stridor and respiratory distress. Urgent chest X-ray AP view (figure 1) showed haziness in the right mid and lower zone. Airway was secured, followed by CECT thorax suggestive of long-segment tracheomalacia with aberrant innominate artery compression. Confirmation was done with a flexible bronchoscope, followed by suctioning to maintain luminal patency. In this article, we report our experience of Tracheomalacia with aspiration pneumonia in the paediatric age group.
Keywords: Stridor, Tracheomalacia, Intrathoracic airway, Brachiocephalic artery, Upper airway obstruction, Flexible bronchoscope, ECAC
Introduction
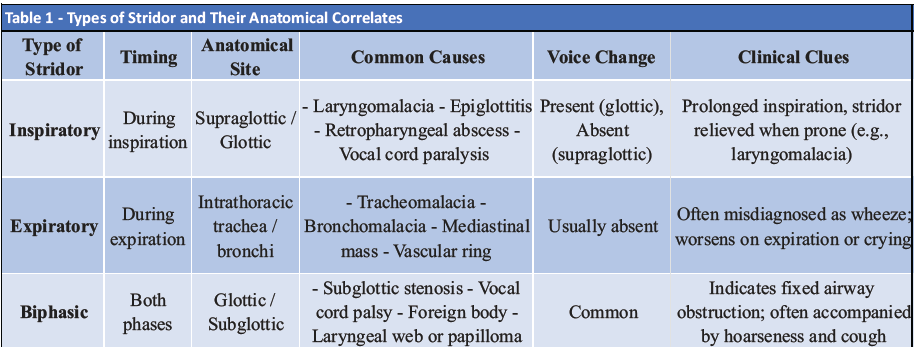
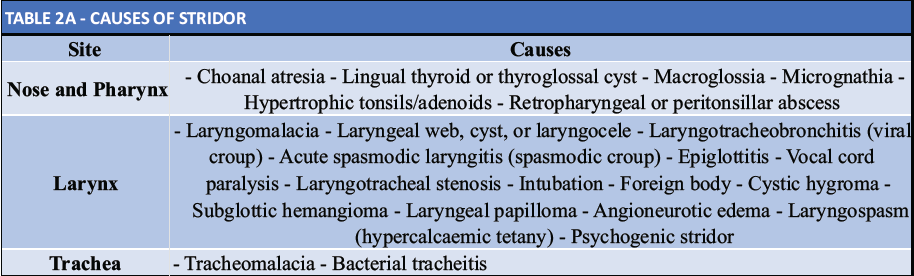
Stridor is a sign of upper airway obstruction. In the paediatric age group, abnormal passage of air through the narrowed airways produces stridor. The cause of stridor can be located anywhere in the extra-thoracic airway (nose, pharynx, larynx, and trachea) or the intrathoracic airway (tracheobronchial tree) (Table 1).
Stridor may be caused by inflammation/infection or inhalation of a foreign body (acute or chronic. It may be congenital or acquired. Laryngomalacia is considered the most common cause of chronic stridor in children younger than two years. It has a male-to-female (M: F) ratio of 2:1 [1]. This may be due to an intrinsic defect or delay in maturation of the supporting structures of the larynx. The airway may get obstructed partially during inspiration due to prolapse of the flaccid epiglottis, arytenoids, and aryepiglottic folds. Inspiratory stridor usually worsens when the child lies in a supine position or when crying or agitated, or when an upper respiratory tract infection occurs [2]. The role of a Critical care physician when faced with an infant with noisy breathing is: (1) to evaluate the severity of respiratory compromise and the requirement for immediate intervention for prevention of respiratory failure; (2) to evaluate the history along with clinical examination to assess whether a significant lesion is suspected and, if so, timely referral of the child to an ENT surgeon for an upper and lower airway bronchoscopy; (3) to evaluate the management strategies of the underlying lesion and to collaborate with other experts for follow-up and further management of the child.
Case Report
A 5-month-old male child was brought to the ER with a history of high-grade fever, which was continuous, associated with chills and rigor for 4-5 days. H/o running nose and cough in the past 1 week. The patient was in respiratory distress with noisy breathing. The mother gives a history of recent history of hospital admission with 15 days of ventilator support and 28 days of hospital admission. Patient was diagnosed with long-segment tracheomalacia with h/o aspiration pneumonia and respiratory failure. The patient had been referred to a tertiary center for further evaluation.
On Examination
A 4 kg child in respiratory distress with HR-155/’ RR-50/’ Temp-103 F, CFT-<3 sec, dehydration present. Saturation on room air was 94-95% On auscultation, B/l crepitations were heard with coarse conductive sounds, and no murmurs were heard. The child was awake but lethargic.
Intervention
Immediately taken on O2 support via nasal prongs (target SpO2->95%), N/G secured.
ABG was suggestive of respiratory acidosis with compensatory metabolic alkalosis.
IV fluids ISO-P @15cc/hr, started on Ceftriaxone 150mg IV BD, Inj Paracetamol and Mefenamic acid for fever control, nebulization with Levo salbutamol (0.31 mg q4hrly) and Budecort (0.5mg q12hrly). Later, colistin nebulisations were added after the culture reports were available.
Urgent chest X-ray AP view (figure 2A) showed haziness in the right lower and mid zone. A lateral view could not be taken. Airway was secured with 3.5no. The ETT and the patient were shifted for urgent CECT thorax (Figure 2B). CECT thorax is suggestive of displacement of the trachea towards the right side. Aberrant origin of the innominate artery (brachiocephalic trunk) on the left side of the Aortic Arch, causing mild anterior indentation/ extrinsic compression on the trachea at the level of the thoracic inlet, s/o possible innominate artery compression of the trachea. Multiple resolving patchy areas of airspace consolidation with surrounding ground glass opacification in the postero basal segments of bilateral lower lobes- possible aspiration pneumonitis.

Bronchoscopy was done using a paediatric bronchoscope, suggestive of long-segment tracheomalacia starting just above the carina.
Investigation
TLC-8100 (N-60/L-35/M-4), NL ratio >3,
Plt-3.84 L, Hb-9.9 gm%, RFT-15.2/0.22, SE-132/4.64, CRP-5.76 mg/dl, ALT-30 IU/l,
Sputum culture- Acinetobacter with intermediate sensitivity only to colistin
Challenges
– Aspiration pneumonia
– Paediatric airway emergency
– Choice of treatment of Tracheomalacia
Procedure
After adequate preparation of the patient and checking the bronchoscope. It is mandatory to keep one size larger and one size smaller than the estimated one. A tracheostomy set is always kept ready for emergency purposes.
Flexible Bronchoscopy was done under sedation (Fig. 2). Pooled secretions were removed, and samples for staining and cultures were sent. Suctioning of intraluminal secretion was performed until the end of the procedure, ensuring clear and confirmed luminal patency.

Discussion
Excessive central airway collapse ECAC is a spectrum of conditions involving abnormal airway collapse >50% of the cross-sectional area during expiration
Two main types (Table 3)
• Tracheobronchomalacia (TBM): cartilage weakness (Figure 3)
• Excessive Dynamic Airway Collapse (EDAC): invagination of the posterior membranous wall with normal cartilage (Figure 3) (Table 4)


Stridor is caused by abnormal air passage during breathing and

is often considered the most prominent sign suggestive of upper airway obstruction. It is usually heard in the inspiratory phase (typically due to supraglottic or glottic obstruction) but may also occur in the expiratory phase (arising from obstruction at or below glottic level and/or due to severe upper airway obstruction). Stridor due to congenital anomalies may present from birth or may develop within days, weeks, or months.
Malacia, derived from the Greek word lakajό (malakos), means softness. Tracheomalacia (TM) is a condition where the walls of the trachea and bronchi develop abnormal flaccidity, leading to collapse of the airway during expiration. Malacia can be confined either to the trachea – tracheomalacia (TM), or bronchi – bronchomalacia (BM), but may also involve the entire airway. Most authors report a male: female (M: F) ratio of about 2:1 in TBM [4]. The loss of airway wall rigidity is most prominent with external compressing forces, as seen during intra-thoracic expiratory effort and is mostly associated with a softening of the cartilaginous architecture of the airway rings or may also present with the congenital absence of supporting rings [3]. (Fig. 4)

The presenting symptoms of airway obstruction present with varying severity. Some children present with stridor, cough, or recurrent chest infections, while some are ventilator-dependent. Signs of tracheomalacia include cyanosis, a prolonged expiratory phase, stridor (which may be biphasic), respiratory distress, and signs of infection. Sternal or intercostal retraction may be apparent when the condition is severe. Respiratory distress usually manifests as grunting, open-mouth breathing, and head retraction. The Common presenting symptoms are summarised in Table 2, which highlights the highly variable nature of this reporting [3].

A chest radiograph can show signs of pneumonia/pneumonitis. The lateral neck radiograph is usually taken with extension of the neck and during the inspiratory phase so that the pharyngeal soft tissues are not confused with a retropharyngeal mass. Computed tomographic (CT) scan and magnetic resonance imaging (MRI) may be obtained to visualize the anatomy of the airway and the surrounding soft tissue structures, including any evidence of vascular compression or anatomical compression.
Direct examination of the airway is often necessary to confirm the diagnosis and is essential in the evaluation of children with persistent stridor. Flexible fibreoptic bronchoscopy is commonly used in the evaluation of airways in children. However, the use of rigid bronchoscopy performed under general anaesthesia (GA) gives a better view of the airway, especially the subglottic view. Rigid bronchoscopy also helps in tissue biopsy and removal of foreign bodies.
A complete blood count is useful if an infection is suspected. Determination of the ESR helps assess the presence of an infection. Depending on the degree of respiratory distress, ABG determination may be necessary to assess the degree of hypoxia and ventilatory status of the patient. An electrocardiogram (ECG) and echocardiogram (2D-Echo) are indicated if significant heart murmurs are present or when structural heart disease is suspected in patients.
Treatment of stridor should be directed to the underlying cause. The airway should be secured immediately in children with severe respiratory distress or actual airway obstruction. This can be done via endotracheal intubation. After adequate ventilation, which is achieved by intubation, tracheostomy may be performed if deemed necessary. Supportive measures like oxygen, humidified air, intravenous fluids, suction, and aerosol treatments with steroids and beta-adrenergic drugs may be used.
Innominate Artery Compression Syndrome
Innominate artery compression syndrome, also known as brachiocephalic artery compression syndrome, is a rare cause of tracheal stenosis that is seen in the paediatric population. Abnormal compression of the anterior aspect of the trachea occurs as the brachiocephalic artery crosses it. Children with age less than 3 years with stridor, breathing difficulties, asthma, apnoeic spells, and recurrent respiratory infections should be suspected of this condition [6]. The brachiocephalic artery usually originates from the left of the trachea in normal children without obstructive symptoms or associated tracheal compression [5]. The artery subsequently impinges/compresses the trachea as it traverses anteriorly at the level of the thoracic inlet [5].
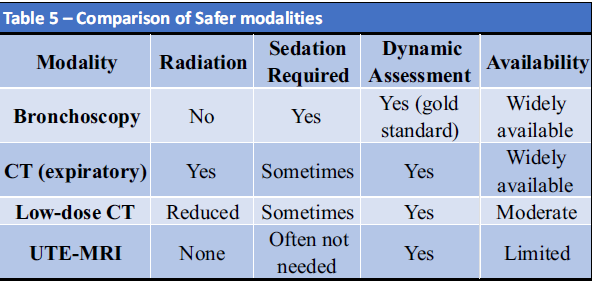
Safer Imaging Alternatives for Diagnosing Tracheomalacia
Background
Traditional diagnostic modalities like dynamic bronchoscopy and CT with expiratory imaging are effective but come with limitations:
• CT scans involve ionizing radiation, which is a concern in Paediatric populations.
• Bronchoscopy requires general anesthesia or sedation, adding risk in unstable or very young children.
Alternative Modalities:
1. Expiratory Low-Dose CT scans
• Offers dynamic assessment of airway collapse during expiration.
• Use of low-dose radiation protocols can reduce overall exposure.
• Fast and accessible, often used in high-suspicion cases when bronchoscopy is not feasible.
Limitations:
• Still involves radiation.
• Often needs sedation in young children.
• Not suitable for serial follow-ups.
2. Ultra-Short Echo Time MRI (UTE-MRI)
What is it?
• A novel MRI technique with very short echo times, allowing for imaging of lung parenchyma and airways, previously difficult with conventional MRI due to low proton density.
Advantages of Tracheomalacia:
• No ionizing radiation – extremely valuable in Paediatric populations.
• Allows dynamic imaging during respiration (free breathing or controlled).
• May eliminate the need for sedation in older cooperative children.
• Offers multi-planar airway visualization similar to CT or bronchoscopy.
• Can assess both airway dynamics and parenchymal abnormalities in the same scan.
Limitations:
• Not yet widely available in all centers.
• Longer acquisition time in some protocols.
• Still under validation in large-scale paediatric studies.
(Table 5)
Treatment Options for Malacia in Children
The treatment plan will be tailored to the individual child, the underlying pathology, the skills and experience of the team, and with a holistic approach to other pathologies and clinical concerns. Tracheostomy is a feasible option where the area of narrowing is confined to a section of the trachea and will be splinted by the tracheostomy shaft, and buy time for natural improvement or surgical repair. Aortopexy – Hitching up the anterior vascular anatomy and attaching it to the back of the sternum (with removal of the thymus) can support the airway. This procedure ideally suits a limited section of malacia following repair of a tracheo-oesophageal fistula. Sleeve resection is done less commonly but can be considered where there is a congenital absence of one or two rings leading to an area of significant malacia. Placement of External Splinting involves a technique where the malacic airway is suspended by sutures to a rigid prosthesis placed around either the affected bronchus or the trachea. Insertion of an Internal Stent. In Candidates for stent insertion, the main indication for stenting is failure of medical and surgical treatments with persistent severe symptoms. In practice, stenting is most often suggested for children who are ventilator dependent and has to date often been considered an intervention of last resort.
Conclusion
Tracheobronchomalacia (TBM) is associated with significant problems for affected individuals, their families, and the clinical team. In the recent literature, the incidence of TBM is probably increasing due to improved survival of premature infants and patients with congenital heart disease and OA/TOF. TBM has been associated with increased morbidity and longer stays in intensive care following surgery for congenital heart disease. Each case is unique and often complex, and patients are best managed by an interdisciplinary team. A stepwise approach to treatment is usually adopted, starting with medical management before consideration of tracheostomy, other surgical options, or stent insertion.
Directions for Future Research
• A better understanding of the underlying pathogenesis for the malacic process to guide the development of growth factors for cartilaginous strength and integrity.
• A paediatric classification for degrees of malacia to assist with further research and management.
• The use of 3D printing to design and print bespoke stents for the growing child.
• The use of bioabsorbable materials for both internal stents and external splints that will have a predetermined absorbable period for use in transient conditions and growing airways.
References
1. Simon NP. Evaluation and management of stridor in the newborn. Clin Pediatr. 1991;30:211-6.
2. Clough J. Managing stridor in children. Practitioner. 1995;239(1557):724-8.
3. Wallis C, McLaren CA. Tracheobronchial stenting for airway malacia. Paediatric Respiratory Reviews. 2018 Jun 1;27:48-59.
4. Masters IB, Chang AB, Patterson L, Wainwright C, Buntain H, Dean BW, Francis PW. Series of laryngomalacia, tracheomalacia, and bronchomalacia disorders and their associations with other conditions in children. Paediatric pulmonology. 2002 Sep;34(3):189-95.
5. Koivikko A, Puhakka H, Vilkki P. Innominate Artery Compression Syndrome. ORL. 1976;38(3):187-92. doi:10.1159/000275274
6. Fawcett SL, Gomez AC, Hughes JA et-al. Anatomical variation in the position of the brachiocephalic trunk (innominate artery) with respect to the trachea: a computed tomography-based study and literature review of Innominate Artery Compression Syndrome. Clin Anat. 2009;23 (1): 61-9. doi:10.1002/ca.20884
| How to Cite this Article: Nair A, Mathew J, Athira CN | The Hidden Collapse: Tracheobronchomalacia as an Overlooked Cause of Paediatric Stridor in the ER | Journal of Anaesthesia and Critical Care Case Reports | May-August 2025; 11(2): 11-16. |
(Article Full Text HTML) (Download PDF)